From Med Students to Rural Hospital CEOs, All Areas of Medicine Are Navigating Through COVID-19
By Stacy Kusler on
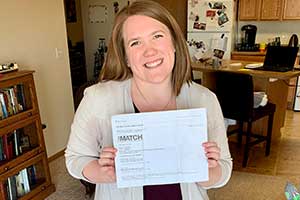
letter at home.
Fourth-year medical student Ashlyn Kamrath was preparing to gather with her classmates, family, and friends on Match Day, a nationally scheduled single-day event when medical students around the country find out if and where they matched to a residency program. Match Day, held this year on March 20, was supposed to be a meaningful celebration of achieving the next milestone on Kamrath's path to becoming a doctor.
Then COVID-19 hit, and the event was canceled just days before it was set to take place.
Stories such as Kamrath's are common these days – life interrupted, plans altered. However, medical education continues, albeit in an adjusted fashion, as does the rest of the health industry, including rural healthcare.
Rural hospitals, like their urban counterparts, are under great financial strain due to the COVID-19 pandemic. They have had to reduce all non-emergent patient visits and scale down services to protect patients and staff. According to Darrold Bertsch, CEO of Sakakawea Medical Center in Hazen and Coal Country Community Health Centers in Beulah, Hazen, Center, and Killdeer, the pandemic is putting a real financial strain on rural hospitals.
Hospitals that have always operated on razor-thin margins are realizing additional challenges with decreased revenues.
"Many rural hospitals find it challenging during the best of times to survive," he said. "Hospitals that have always operated on razor-thin margins are realizing additional challenges with decreased revenues."
Bertsch, who also collects annual financial data from all 36 Critical Access Hospitals (CAHs) in the state, says that about half of North Dakota CAHs have a positive operating margin on a normal year.
"Certainly, through this, more hospitals will report a negative operating margin," he said.

equipment.
In addition to reducing patient visits, such providers have also stopped training medical students at their facilities for the sake of both patient and student safety. This has affected rural facilities in a negative way in so far as such training experiences are a great recruitment tool.
The stoppage certainly affects the students, too.
Third-year medical student Audrey Lane was in the midst of her Rural Opportunities in Medical Education experience in Jamestown, where she had been training since December. Through this rural immersion program, she was learning valuable hands-on patient care. Her training was set to wrap up in mid-June, but the pandemic changed her training from in-person to virtual.
I've seen patients for pre-op visits, prenatal visits, or even starting a new medication, and it's disappointing not to see how this care will continue.
"I chose this experience for the chance to follow the same patients over an extended period of time," Lane said. "This has been one of the more disappointing parts of having my rotations stalled by COVID-19. I've seen patients for pre-op visits, prenatal visits, or even starting a new medication, and it's disappointing not to see how this care will continue."
Additionally, missing clinical experiences is making it harder to decide confidently on the specialty in which Lane eventually wants to practice.
"With the shift to remote learning, I'll have to rely on the experience I've already had, and self-reflection, to develop that confidence for which residency I'll apply to," she said.
Brighter Days Ahead
For Pete Antonson, CEO of Northwood Deaconess Health Center in Northwood, the pandemic could forever change the way his team approaches patient care, but not necessarily in a bad way.
"With so many asymptomatic people, I think this will make us more defensive in our day-to-day activities of caregiving, particularly in the areas of hospital and clinic, beyond the pandemic," Antonson said.
Northwood Deaconess also operates a nursing home on campus, a division of healthcare that has been on high alert since the beginning of the pandemic due to the high-risk nature of the virus to older individuals. Like many other nursing homes, Northwood Deaconess Nursing Home has had more one-on-one interactions between staff and residents (versus group activities), and technology has been used more frequently to connect residents to friends and family while maintaining social distance.
"I think we have learned, in the nursing home, the great benefit of these types of interactions, such as FaceTime and Skype," Antonson said, noting that geographical barriers that may have prevented family visits before are now no longer really a barrier at all with the increased comfort people have with technology.
Help is also on the horizon for rural North Dakota hospitals. In late April, the Health Resources & Services Administration announced a grant for special crisis funding through the Coronavirus Aid, Relief, and Economic Security (CARES) Act. This funding was awarded to the Small Rural Hospital Improvement Program program at the University of North Dakota Center for Rural Health, which will be the mechanism for distributing funds to rural North Dakota CAHs. Just more than $71,000 will be available for reimbursement for each of the 36 CAHs in the state as they prepare for and respond to the COVID-19 pandemic during the next 18 months. Rural hospitals were also able to take advantage of other funding opportunities through the CARES Act, as well as the Paycheck Protection Program.
Lemons from Lemonade
Even though her planned Match Day celebration was canceled, Kamrath, a Lakota, North Dakota, native, still found a way to virtually celebrate her milestone with her loved ones, and she was thrilled to receive news that she matched to her first choice of residency through Altru Family Medicine Residency in Grand Forks. While she wraps up her medical school career online, rather than in-person, she is still scheduled to begin residency training this summer. Kamrath, who hopes to practice rural family medicine someday, said, "There are always nerves present when preparing for something new, especially the transition into residency. The COVID-19 pandemic is definitely adding uncertainty."
I think this pandemic has in ways forced change in the practice of medicine, the teaching of medicine, and how we all live in general.
While it may be easy to focus on the negatives right now, Kamrath is instead choosing to look on the bright side. "I think this pandemic has in ways forced change in the practice of medicine, the teaching of medicine, and how we all live in general," she said. "It has also fostered improvisation, ingenuity, and adaptability, which are key in the practice of medicine, especially rural medicine."


 is the connection between rural healthcare facilities in North Dakota and qualified health professional job seekers. As the workforce specialist, she assists rural facilities to attract medical providers and other health professionals to their communities by sharing job opportunities. Through her position, Stacy is working to reduce the healthcare workforce shortages throughout the state.
is the connection between rural healthcare facilities in North Dakota and qualified health professional job seekers. As the workforce specialist, she assists rural facilities to attract medical providers and other health professionals to their communities by sharing job opportunities. Through her position, Stacy is working to reduce the healthcare workforce shortages throughout the state.



